Antibiotics have been increasingly used not only to treat humans and animals but also for crop protection as pesticides. Thus, antibiotics and pesticides can coexist in certain environments. To investigate the impact of co-occurring non-antibiotic pesticides on the development of antibiotic resistance, researchers conducted long-term exposure experiments using an Escherichia coli K-12 model strain.
The results show that pesticide exposure alone led to the emergence of mutants with significantly higher levels of resistance to streptomycin; whereas pesticide exposure with a subinhibitory level of ampicillin synergistically stimulated the emergence of ampicillin resistance and cross-resistance to other antibiotics (e.g. ciprofloxacin, chloramphenicol and tetracycline).
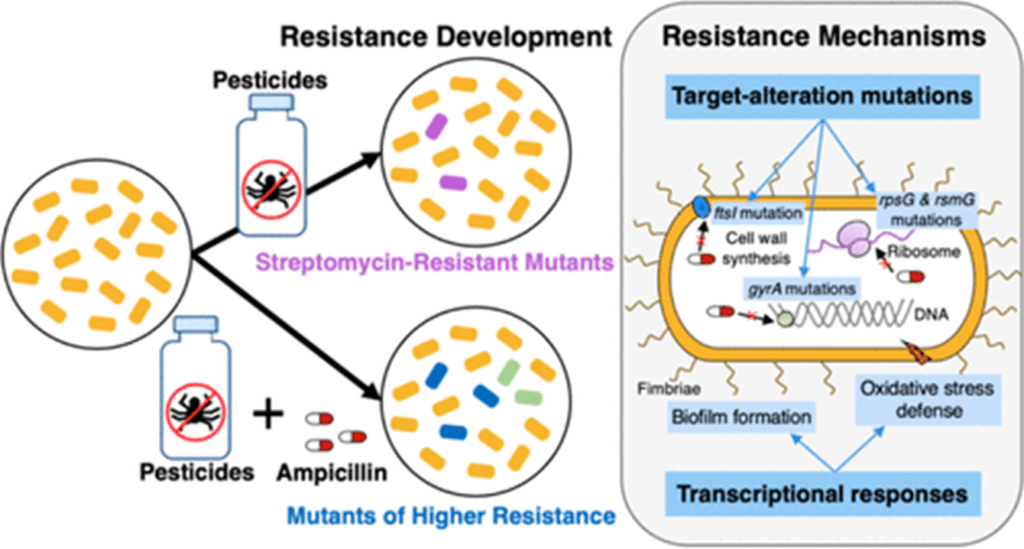
The combined exposure to pesticides and ampicillin has resulted in different and diversified genetic mutations in resistant mutants. The genetic mutations likely caused holistic transcriptional regulation (e.g. biofilm formation, oxidative stress defence) when grown under antibiotic stress, leading to increased antibiotic resistance.
Together, these findings provide important insights into the development of antibiotic resistance and the mechanisms of resistance in environmentally relevant settings where antibiotics and non-antibiotic micropollutants coexist.
New mechanisms of antimicrobial resistance are emerging and spreading worldwide, threatening our ability to treat infectious diseases. At the same time, pesticide use is increasing worldwide: between 1990 and 2019, average pesticide used per area of cropland increased from 1.55 to 2.69 (kg/ha).
Recent evidence shows that AMR can also occur in natural environment - as a result of multiple interactions between livestock and soil and water contaminated with chemicals commonly used in agriculture. Resistant bacteria from altered environments can become a major public health problem. The role of pesticides in the development of resistance in different bacteria has been previously investigated, for example Forsberg et al, 2012 or Rangasamy et al, 2017.
Bacterial biopesticides can also contribute to the development of resistance. A new study investigated a biopesticide containing Bacillus thuringiensis-t (Bt). Bacillus thuringiensis-t is a soil-dwelling bacterium that produces a toxin that is lethal to certain herbivorous insects. This toxin has been used as an insecticide for about 100 years and is also commonly used in organic farming and as a substitute for DDT. Bt is also the source of the genes used to genetically modify some food crops to produce the toxin themselves to repel pests. Because Bt is closely related to bacteria that can cause human illnesses, there is a risk that if Bt sprayed as an insecticide carries resistance genes, it could pass these on to human pathogens living in the soil. The researchers sequenced the genomes of Bt bacteria and found that they are resistant to a number of antibiotics, including tetracycline, ceftazidime, cefazolin and ertapenem.
Given the seriousness of the problem of AMR, it is a topic worthy of further research. The case also highlights the importance of the One Health approach, which recognises that human health is linked to the health of animals and the environment. Understanding the interrelationships between soil, water and pesticides is essential to raising awareness of the need for environmental monitoring programmes and to addressing the current crisis of AMR.
